Status Quo Maintained: FDA Reverses Course on Generic Product Labeling
by Chad Landmon and Eric Dunbar 
Enacting another reversal of a policy proposed during the Obama administration, on December 13, 2018, FDA announced its withdrawal1 of a rule proposed in 20132 that would have permitted generic drug manufacturers to revise their product safety labels to reflect newly acquired information through a “changes being effected” (CBE-0) supplement—a procedure previously only available to new drug application (NDA) holders. Many patient advocacy groups and plaintiffs product liability lawyers advocated for the proposed rule because permitting abbreviated new drug application (ANDA) holders to alter their product safety labeling prior to FDA review and approval of the revised label may have exposed ANDA holders to “failure to warn” product liability suits. In addition to tort liability exposure, the rule would have effectively required generic manufacturers to greatly expand their internal reporting systems, tracking systems, and medical expertise to implement the necessary labeling changes. Given the burden the rule would have imposed and the potential confusion to patients from having different labels for generic and branded products, FDA decided to withdraw this rule.
Withdrawal of this proposed rule will undoubtedly be cheered by the generic drug industry because it should eliminate lingering concern over potential failure to warn tort liability and maintain the status quo for product labeling. That being said, FDA at the same time announced that its fiscal year 2019 Budget Request includes a request for resources to update generic drug labeling in instances where the original brand product has been discontinued or withdrawn for reasons other than safety or efficacy. Depending upon where FDA goes with this effort and whether FDA puts some onus on generic manufacturers in instances where the brand product is no longer being marketed, generic manufacturers may be back in the crosshairs of product liability lawyers and may have to once again plan to invest resources in enhanced monitoring, reporting and medical evaluation systems.
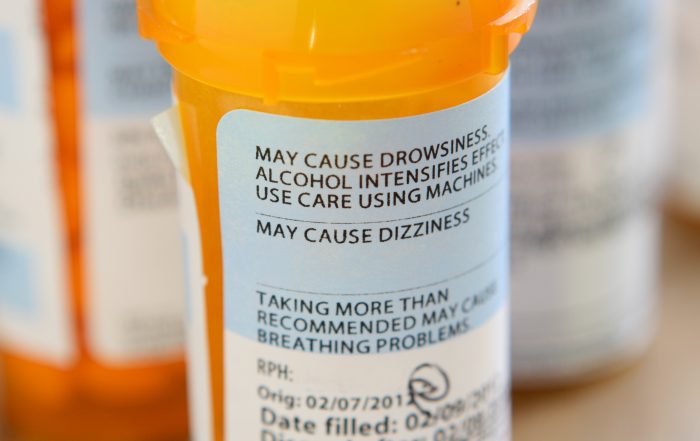
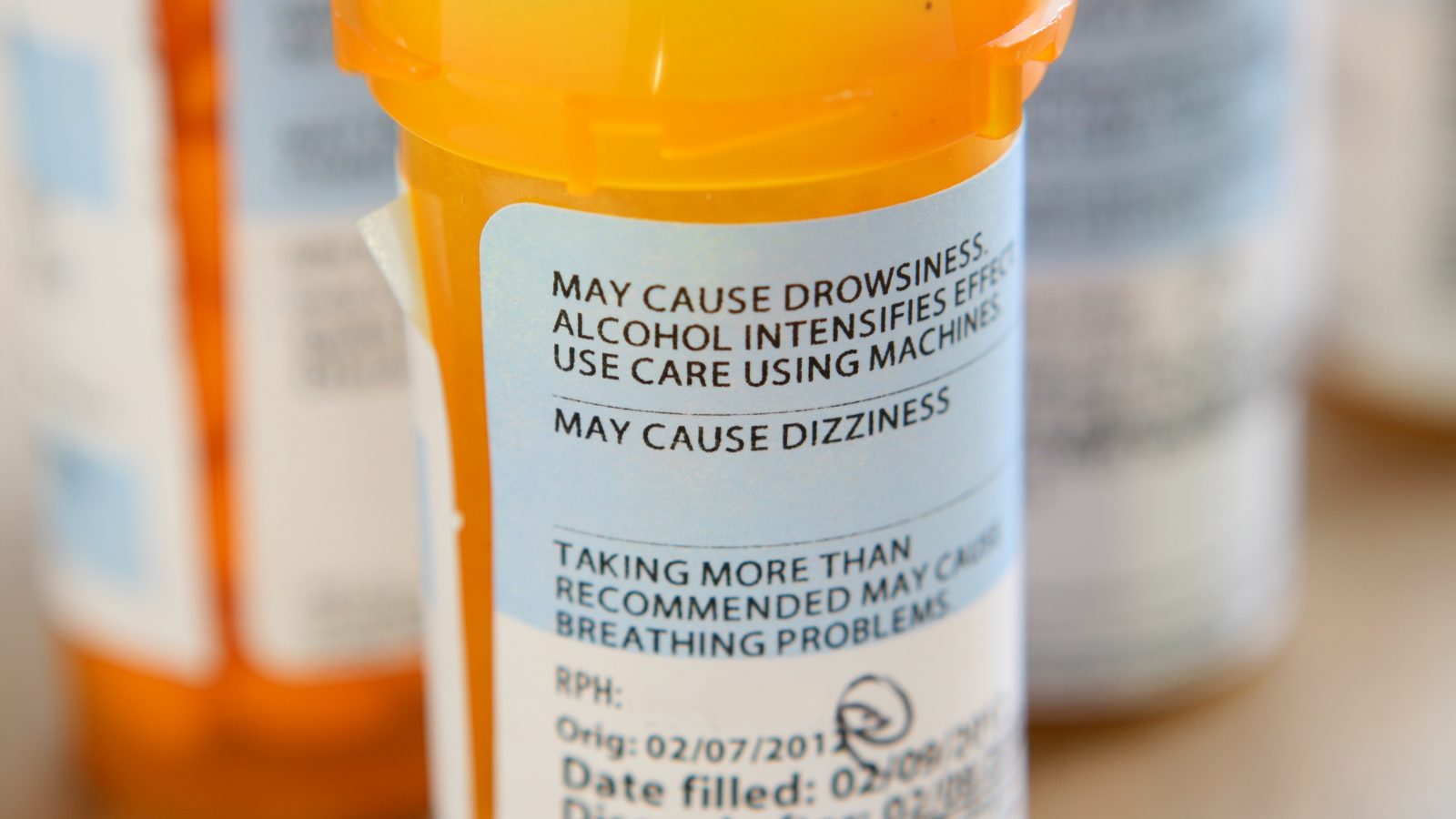
Postapproval Safety Label Regulations
All NDA and ANDA holders are required to develop procedures for the surveillance, receipt, and evaluation of postapproval adverse drug experiences to FDA.3 Application holders must also comply with postapproval reporting requirements, which include submission of an annual report to FDA. Annual reports should include a summary of newly acquired information that might affect the safety, efficacy, or labeling of the drug product and proposed revisions to the product’s label to accommodate for the information received from postapproval drug experiences. Once an application holder is aware of information rendering its label inaccurate, the holder has an ongoing obligation to resolve the disparity between its labeling and the most accurate safety information.4
Most substantive changes to a product’s labeling must be submitted by the application holder through a prior approval supplement, which FDA must approve before the holder is permitted to implement the change. However, FDA permits certain labeling changes based on newly acquired postapproval information to be implemented immediately upon submission of a CBE-0 supplement to FDA at the time of distribution.5
These labeling changes broadly include many categories of safety information about a drug product.6 After a CBE-0 supplement is submitted, the application holder may revise the product’s label to reflect information submitted in the supplement while FDA review is pending. FDA proceeds to review all information submitted in the CBE-0 supplement, including any proposed labeling change and the underlying data supporting the proposed change, and then either accepts, rejects, or requests a modification to the proposed change. The purpose of the CBE-0 supplement is to allow application holders to promptly update drug safety information when they become aware of such information in order to better inform prescribers and consumers, while maintaining FDA oversight.
Generic drug manufacturers, on the other hand, are required to maintain the same safety labeling as the generic drug’s reference listed drug (RLD).7 Accordingly, only NDA holders may submit CBE-0 supplements to substantively change a drug product’s safety labeling to reflect postapproval, newly-acquired information. If an ANDA holder acquires postapproval information through its required surveillance procedures that may affect the safety of the drug product, and the ANDA holder believes such information should alter the product’s labeling, the ANDA holder may not independently update its safety labeling or submit a CBE-0 supplement. The ANDA holder must instead submit the newly-acquired information to FDA through a prior approval supplement, and FDA will subsequently decide whether the labeling for the drug product, both for the RLD and the generic version, should be revised.8 An ANDA holder may not unilaterally alter its product label to reflect postapproval information and may only submit a CBE-0 supplement to effect a label change that conforms to the RLD or in response to a specific request from FDA.9
These postapproval safety label regulations and revision procedures—specifically, the difference between how NDA holders are permitted to alter a drug product’s safety label versus how ANDA holders are permitted to—create the product liability framework addressed by the Supreme Court in Wyeth v. Levine10 in 2009 and Pliva, Inc. v. Mensing11 in 2011.
Preemption and Product Liability
In Wyeth v. Levine, Levine brought a state tort law claim against Wyeth alleging “failure to warn” product liability. The product at issue in Levine was injectable Phenergan, an anti-nausea medication first approved by FDA in 1955. In 1973 and 1976, Wyeth submitted supplemental new drug applications for Phenergan, which FDA cleared following proposed labeling changes. In 1981, Wyeth submitted a third supplemental application in response to a new FDA rule governing labels. Wyeth corresponded with FDA multiple times regarding Phenergan’s label. Notably, in 1987, FDA suggested amendments to Phenergan’s label with respect to the risk of arterial exposure. Wyeth submitted a revised label incorporating FDA’s proposed changes in response, but FDA did not respond. In 1996, FDA instructed Wyeth to “retain verbiage in [the] current label” regarding intra-arterial injection. Finally, in 1998, FDA approved the 1981 supplemental new drug application and instructed Wyeth that the label “must be identical” to the approved package insert. In 2000, Levine was injected with Phenergan, which caused the onset of gangrene—tissue death due to lack of blood supply—and amputation of her forearm and hand.12
Levine argued that Wyeth, an NDA holder, was liable for state law product liability for Phenergan, which caused her adverse event, because the product’s labeling did not include adequate warnings. Although Phenergan’s label warned of gangrene and amputation following inadvertent intra-arterial injection, Levine argued that the labeling was defective because it failed to instruct clinicians to use one method of administration over a higher-risk method of administration that is more likely to result in these adverse events. In response, Wyeth argued that it was impossible to comply with both state and Federal regulations governing postapproval drug product labeling because it could not have modified the drug product’s label without first obtaining FDA approval of such changes. Further, FDA has specifically required this allegedly defective label in its approval of Phenergan’s application.
Wyeth argued that because it was impossible for it to comply with both state tort law and federal labeling regulations, it could not be liable under state tort law because the claim is preempted.13 The Supreme Court held that it was not impossible for Wyeth to comply with both state and federal laws because, as an NDA holder, Wyeth could have submitted a CBE-0 supplement to unilaterally revise the drug product’s label to adequately warn consumers and prescribers of such adverse events without FDA approval.14 Consequently, Wyeth was held liable under a “failure to warn” theory of product liability for inadequacies in the drug product’s safety label.
Levine clearly held that NDA holders may be liable under a “failure to warn” theory of product liability for inadequate drug labeling where the application holder could have revised the labeling through a CBE-0 supplement to adequately warn of adverse events the application holder became aware of through postapproval surveillance and evaluation procedures. Following Levine, ambitious litigants sought to extend similar reasoning to expose ANDA holders to the same liability. Over the following two years, many courts agreed with these ambitious litigants.15
In Pliva, Inc. v. Mensing, the Supreme Court took up the question of whether ANDA holders could be held liable under this theory. The Court held that an ANDA holder may not be held liable under a state law “failure to warn” theory of product liability for inadequate labeling where the safety information was derived from postapproval adverse events because the state tort law claim was preempted by federal law, such that it would be impossible for ANDA holders to comply with both.16 Unlike NDA holders, ANDA holders were not permitted to unilaterally revise labeling to reflect newly-acquired information without FDA approval, and ANDA holders were required to maintain the same labeling as the RLD. Therefore, federal law required an ANDA holder to receive approval from FDA to revise safety labeling in response to newly-acquired information, which foreclosed the ANDA holder from also complying with state tort law requirements relating to the adequacy of the product labeling.
In the wake of Mensing, patient advocacy groups and plaintiffs product liability lawyers strongly disagreed with the policy this ruling created. From the patient advocacy perspective, Mensing appeared to promote a system that discouraged ANDA holders from promptly collecting, evaluating, and reporting postapproval adverse drug experiences to FDA and promoted a system where outdated and potentially harmful drug product labels remained on the market for a period of time. This was especially so considering that around 80% of prescriptions were being filled with generics during this period.17 In addition, plaintiffs tort lawyers and patient advocacy groups argued that the Supreme Court’s decision was unfair in that it largely shielded generic drug companies from failure-to-warn suits.
In response, Public Citizen filed a citizen petition with FDA in August 2011 to revise its regulations to permit ANDA holders to unilaterally alter their products’ labeling through a process similar to that available to NDA holders, which would expose ANDA holders to similar liability.18 Public Citizen is a nonprofit consumer advocacy organization that has advocated for and litigated many public interest cases, in addition to frequently petitioning FDA for issues related to consumer and product safety.19 Following submission of this petition, multiple parties commented on the petition over the following two years.20
The Proposed Rule
In November 2013, in response to Public Citizen’s petition and the Mensing decision, FDA proposed a new rule that would permit ANDA holders to unilaterally revise and distribute drug products’ safety labeling that may differ from the RLD in response to newly acquired safety information.21 In relevant part, this proposed rule would have permitted ANDA holders to effect labeling changes by submitting a CBE-0 supplement, in the same manner that NDA holders are permitted to.
In support of this proposed rule, FDA cited “ensur[ing] that generic drug companies actively participate with FDA in ensuring the timeliness, accuracy, and completeness of drug safety labeling.”22 In addition, FDA explicitly noted that the proposed rule “may eliminate the preemption of certain failure-to-warn claims with respect to generic drugs.”23
FDA further recognized that this proposed rule may have resulted in temporary differences between labels for the same drug product, both between the RLD and generics and between different generic alternatives, while FDA review of CBE-0 supplements was pending. These discrepancies may have caused significant prescriber and consumer confusion and under-mined consumer confidence in the efficacy and therapeutic equivalence of generics. To ameliorate any confusion caused by differences, FDA proposed creating a webpage that it would maintain “on which FDA would promptly post information regarding the labeling changes proposed in a CBE-0 supplement while FDA is reviewing the supplement.”24 This webpage would include all the necessary information about the CBE-0 supplement under review including, in relevant part, the drug product, the pre-supplement label, the proposed changes, and the sources submitted in support of the proposed changes.
Following this proposal, FDA accepted comments from interested parties, and the proposed rule remained pending for over five years. FDA received many diverse comments in favor of approval or withdrawal of the proposed rule, many of which cited the reasons discussed by FDA in its proposal. In addition, FDA held a public meeting in March 2015 that allowed any interested stakeholder to advocate its argument for or against the proposed rule or any alternative proposal directed at the same goal.25
FDA Changes Its Mind
FDA decided to withdraw the proposed rule on December 13, 2018.26 In its withdrawal, FDA cited many of the potential externalities raised in its proposal, which were amplified during the comment period.27
In support of the proposed rule, FDA acknowledged comments that argued the proposed rule “would enhance drug safety by making healthcare practitioners and the public aware of new safety-related information about a drug more quickly.”28 This support spoke to FDA’s original purpose for proposing the rule. Further, stakeholders in favor of the proposed rule acknowledged that, although it may impose tort liability on generic manufacturers, such liability “may be an incentive for drug manufacturers to ensure that their product labeling reflects the most current safety information.”29
Stakeholders in favor of the proposed rule succumbed to a flood of comments in strong opposition. First, FDA noted comments opposing the proposed rule, which stated that “generic drug application holders do not generally receive or possess all the data necessary to evaluate postmarket safety in-formation and to support safety-related labeling changes.”30 As noted above, all application holders do currently have certain postapproval surveillance, receipt, evaluation, and reporting requirements. ANDA holders, however, are not required to independently recreate all the medical safety data collected by NDA holders during the initial approval process for a new drug product. ANDA holders maintain a significantly reduced capacity to independently research and evaluate safety risks compared to NDA holders. If this proposed rule had been implemented, bringing ANDA holders’ safety label revision requirements in parity with NDA holders’ requirements would have placed a significant burden on generic manufacturers to both develop and maintain similar reporting mechanisms, well beyond what they currently have the requirement or capacity to handle.
Further, FDA acknowledged comments in opposition to the proposed rule affirming concerns FDA raised in its proposal about prescriber and consumer confusion, as well as casting doubt on the therapeutic efficacy of generics.31 Both these factors may lead consumers and prescribers to rely on generic alternatives less, which would significantly undermine the generic market and the structure of the public health system, which permits generic alternatives to promote accessibility. Finally, FDA acknowledged that “most concerns regarding [the] economic impact” of this proposed rule focused on the “increased risk of tort litigation against generic drug manufacturers.”32 Exposure to “failure to warn” product liability would necessarily force generic manufacturers to increase prices on their drug products, as the cost of defending a multitude of failure to warn product liability cases would have to be absorbed by generic manufacturers by passing it off to the consumer.
After evaluating these competing comments, FDA concluded that, although the proposed rule would further its goal of “ensur[ing] that generic drug labels reflect up-to-date, science-based information to inform patients and providers,” the negative externalities of this proposed rule would place so significant a burden on generic manufacturers as to prohibitively discourage “a pathway for the development of generic drugs that is modern, efficient and low cost.”33 In balancing these competing goals, FDA determined that this proposed rule would have “compromise[d] public health.”34
Aftermath
Upon withdrawal of the proposed rule, and absent any change in legislation or case law governing postapproval drug safety label revisions, ANDA holders are only permitted to revise safety labels through the same supplement processes available prior to the proposal of this rule, as described above. Although FDA ultimately did not alter safety label regulations, proposal of this rule raised an important debate about how to best communicate the most accurate safety information to consumers and prescribers. FDA has stated that it “is actively evaluating [alter-native] ways to facilitate the updating of generic drug labeling” without imposing prohibitive barriers to a large portion of the drug market.35
To that end, concurrent with its withdrawal of the proposed rule, FDA announced that its fiscal year 2019 Budget Request “includes an investment to support efforts to update generic drug labeling, with an initial focus on oncology products.”36 FDA identified 1,170 RLDs (out of a total of 5,600 that are tied to generic alternatives) that have been discontinued or withdrawn by brand manufacturers for reasons other than safety or efficacy.37 The generic alternatives for these drug products are at particular risk for maintaining out-of-date safety labels, as the brand manufacturer with the primary resources and responsibility to update the label no longer is making investments in furtherance of the drug product. In effect, these “drug labels become frozen in time” when the brand manufacturer exited the market.38 Through this new initiative, although lacking definition as of now and unfunded, FDA takes it upon itself to research these drugs and update their safety labels. As FDA stated, it will begin with oncology products, as an important subset of the 1,170 brand-abandoned drugs “form the back-bone of modern cancer regimens.”39 It will be important to see whether FDA receives the necessary funding for this initiative and to evaluate any alternative proposals FDA sponsors to encourage safety labeling updates.
In the meantime, FDA’s withdrawal of the proposed rule appears to have maintained the status quo for drug labeling. Generic drug companies have been given a reprieve from the increased demands and potential product liability exposure that would have been imposed if the proposed labeling rule had been made effective. Only time will tell how long the status quo will be maintained.
Update Magazine
February/March 2019
- Withdrawal of Proposed Rule on Supplemental Applications Proposing Labeling Changes for Approved Drugs and Biological Products, 83 Fed. Reg. 64,299 (Dec. 14, 2018); Press Release, Food and Drug Admin., Statement from FDA Commissioner Scott Gottlieb, M.D. and Director of FDA’s Center for Drug Evaluation and Research Janet Woodcock, M.D., on Efforts to Modernize Generic Drug Labels While Maintaining the Efficiency of Generic Development (Dec. 13, 2018) (available at https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm628339.htm).
- Supplemental Applications Proposing Labeling Changes for Approved Drugs and Biological Products, 78 Fed. Reg. 67,985 (Nov. 13, 2013) (proposed rule).
- See 21 C.F.R. § 314.80(b); 21 C.F.R. § 314.98(a); 21 C.F.R. § 600.80(b).
- Applicant holders must update labeling in accordance with 21 C. F.R. § 314.70, 21 C.F.R. § 314.97, and 21 C.F.R. § 601.12.
- See 21 C.F.R. § 314.70(c)(6)(iii); 21 C.F.R. § 601.12(f)(2); Guidance for Industry: CMC Postapproval Manufacturing Changes to be Documented in Annual Reports (https://www.fda.gov/downloads/Drugs/…/Guidances/UCM217043.pdf).
- These changes include: adding a contraindication, warning, precaution, or adverse reaction of the drug product; adding a statement as to the product’s abuse, dependence, psychological effect, or overdosage; adding instructions about dosage or administration intended to make the product safer to use; and removing false, misleading, or unsupported indications.
- See 21 C.F.R. § 314.150(b)(10).
- 57 Fed. Reg. 17,950, 17,961 (Apr. 28, 1992).
- See 21 C.F.R. § 314.150(b)(10); Supplemental Applications Proposing Labeling Changes for Approved Drugs, Biologics, and Medical Devices, 73 Fed. Reg. 2848, 2849 at n.1 (Jan. 16, 2008) (proposed rule); 57 Fed. Reg. at 17961.
- 555 U.S. 555 (2009).
- 564 U.S. 604 (2011).
- 555 U.S. at 559-63.
- Preemption is a legal theory that stems from the Supremacy Clause of the U.S. Constitution (U.S. Const. art. VI § 2) that applies when a state law and Federal law conflict. When this occurs, the Supremacy Clause instructs that Federal law is supreme and displaces state law. Therefore, when faced with a direct conflict, a state law claim is preempted because it is impossible to comply with both state and Federal law, and a tortfeasor cannot be held liable for non-compliance with the state law. See, e.g., Fl. Lime & Avocado Growers, Inc. v. Paul, 373 U.S. 132, 142-43 (2002) (describing preemption where compliance with both state and Federal regulations is a “physical impossibility”); Am. Tel. and Tel. Co. v. Cent. Office Tel., Inc., 524 U.S. 214, 227 (1998) (describing preemption where there is a direct conflict between state and Federal law).
- 555 U.S. at 581.
- See, e.g., Demahy v. Actavis, 593 F.3d 428 (5th Cir. 2010); Mensing v. Wyeth, Inc., 588 F.3d 603 (8th Cir. 2009).
- 564 U.S. at 626.
- See, e.g., Katherine Eban, Are Generics Really the Same as Brand-ed Drugs?, Fortune (Jan. 10, 2013), http://fortune.com/2013/01/10/are-generics-really-the-same-as-branded-drugs/; Scott Hensley, 3 in 4 U.S. Prescriptions Are Now For Generic Drugs, Nat’l Pub. Radio (Apr. 20, 2011), https://www.npr.org/sections/health-shots/2011/05/16/135538006/3-in-4-prescriptions-are-now-for-generic-drugs.
- Sidney M. Wolfe et al., Citizen Petition, Public Citizen (Aug. 29, 2011), https://www.citizen.org/sites/default/files/1965.pdf.
- Accomplishments, Public Citizen, https://www.citizen.org/about/accomplishments.
- See Letter from Janet Woodcock, Dir., Center for Drug Eval. And Research, to Sidney M. Wolfe, Dir., Public Citizen Health Research Group (Nov. 8, 2013) (No. FDA-2011-P-0675).
- 78 Fed. Reg. at 67,989-94.
- Id. at 67,989.
- Id.
- Id.
- 80 Fed. Reg. 8577.
- See supra at n. 1.
- 83 Fed. Reg. at 64,300-01.
- Id. at 64,300.
- Id.
- Id. at 64,301.
- Id.
- Id.
- Press Release, supra at n. 1.
- Id.
- 83 Fed. Reg. at 64,301.
- Id.
- Press Release, supra at n. 1.
- Id.
- Id.